By Kate Pounds
May 9 2020, 09.25
Follow @SW_Londoner
People risk becoming critically unwell as they wait too long to be seen for serious conditions amid coronavirus confusion, according to doctors from many areas of medical practice.
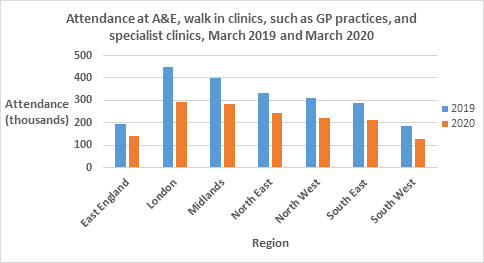
This comes as the NHS launched Help Us Help You, a campaign reminding the public to seek urgent help if they need it, with NHS England estimating attendance at Accident and Emergency was 50% lower in April 2020 than April 2019.
“I felt so sad when I heard an elderly patient who had delayed coming into hospital say they thought the NHS was no longer treating old people,” an experienced accident and emergency registrar in the south east said.
“I’ve been concerned about how quiet our A&E department is for weeks, and sad about elderly people, and others, at home believing they can’t get help.”
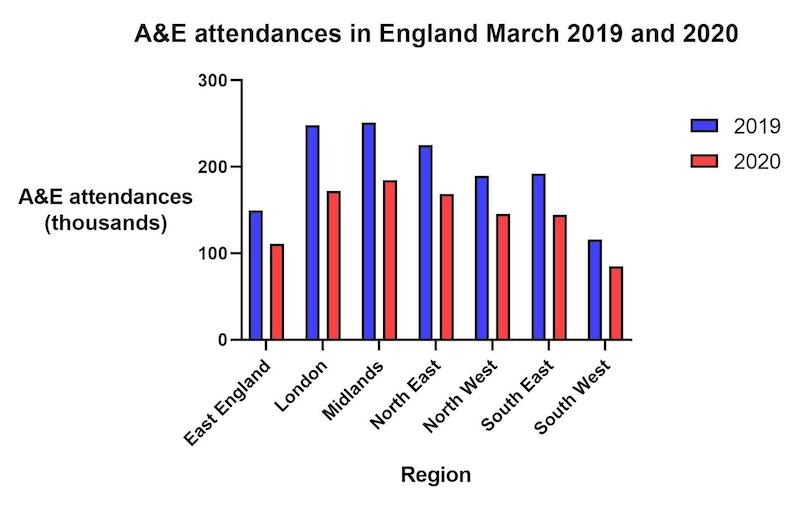
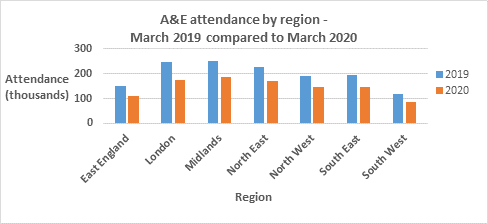
The NHS England data also shows attendance in Accident and Emergency departments was 29% lower in March 2020 than in March 2019.
The doctor, who wished to remain anonymous, explained patients of all ages are waiting and coming to hospital much sicker than usual, and the number of patients coming in with heart attack, stroke, and other serious conditions is very low.
This is backed up by statistics from the British Heart Foundation that show the number of people attending Accident and Emergency departments with symptoms of a heart attack was 50% lower than expected in April 2020.
This doctor felt some elderly people not being ventilated, and messages to stay home and protect the NHS, may have been confused so elderly people thought they wouldn’t be treated at all.
The doctor explained many colleagues from various specialisations around the country are worried by things they are seeing and patients have said to them.
Some have posted on social media, and written to politicians for help.
“We still want to see you, so if you feel unwell, or you are caring for someone and you have concerns about their health, please still contact your GP or call an ambulance in the way you usually would,” the doctor said.
“In A&E we have plenty of space and staff to see and treat people, and a well set up system to separate non-Covid from Covid patients. We will do everything we can to minimise risk to you.”
A consultant anaesthetist from the north west was ‘really worried’ to see a patient needing immediate surgery after staying home for three weeks with appendicitis.
She said: “I’m devastated that parents worried about their children don’t think they can get any help, and patients may be at home too frightened to come to hospital, feeling they wouldn’t be seen and treated because they’re too old or they have too many other problems, that breaks my heart because it’s just not true.”
She heard someone didn’t want to burden the NHS by taking a relative who suffered a minor stroke to hospital and another believed hospital wouldn’t treat a relative with Covid and heart disease.
She thinks opinions have been informed by stories about over-run hospitals in Italy and Spain unable to treat patients in certain groups.
In the UK decisions about intensive care are still made on an individual basis, she explained.
“I think some people are afraid of coming to hospital and dying alone,” she said.
“We have people who sit with them and hold their hands, and doctors FaceTime relatives on iPads, but it is devastating when family can’t be there to say a proper goodbye.”
Other doctors she spoke to share her concerns.
She wrote to Jeremy Hunt, chair of the Health Select Committee.
“I wanted to inform the government that things are okay and we are coping,” she said.
She added: “We don’t want people to think there’s nothing to worry about, Coronavirus is deadly to some people and sometimes apparently randomly.
“Lockdown has flattened the peak, it’s absolutely 100% vital that people stay at home to protect the NHS
“For various reasons before Covid people were coming to A&E who didn’t need to be there, and we’re grateful for a reset, but we want people who would benefit from hospital to come in.
“Please come and seek help if you need it, We’ll get you home as soon as we can, and we’ll do our very best to protect you from Covid.”
A GP from the south said: “I think we are seeing more things that would normally go to A&E, such as patients with injured limbs so severely painful and swollen they can’t move them, and people much sicker because they have waited longer than usual before coming in.”
Four in ten people say they wouldn’t visit the GP at the moment for fear of burdening the NHS, data from NHS England shows.
Another GP said they speak to many patients daily who have put off calling and believe they are wasting doctors’ time. Some fear Covid and refuse to go to hospital, and others need “serious persuasion.”
An obstetrics and gynaecology doctor from the west Midlands said: “I’m worried about potential still-births as patients in antenatal clinics with pregnancy concerns such as reduced movements, pain or bleeding, are avoiding hospital.
“They worry about catching Covid, and assume we’ll be too busy to see them.
“I just keep repeating that we still want them to call and come in.”
Matt Wicks, 38, a teacher from Oxfordshire, who had a major operation after waiting more than two days at home with severe stomach pain, explained he wishes he had sought help sooner. He said: “What I had is normally a 24-hour job, but this was 12 days in hospital with no visitors and weeks of recovery at home.”
“They did everything they could to protect me from Covid and I felt safe, and they never gave me the impression I was overburdening them.
“Obviously you’re at higher risk there than you are at home on your sofa, but if you think you have something serious you’ve got to get it checked out.”
Age UK charity director Caroline Abrahams said people of all ages may not know of measures to separate patients in hospitals and lots of older people are confused about the advice to them.
“Stay home save lives is working really well,” she said. “We don’t want to confuse that, but people with serious illness should still go to hospital or ring their GP for advice, and don’t assume something non-Covid won’t get treated because it really will.”
The NHS campaign, Help Us Help You, launched on April 25, includes digital adverts, posters and social media.
NHS chief executive Sir Simon Stevens said: “Seek help in the way you always would.
“Ignoring problems can have serious consequences.”




